If we had a dollar for every time a patient asked us if the pill was going to make her fat, we might be able to double our salaries. Myths about contraception are all too prevalent and continue to be a barrier to providing contraception for our patients. Unfortunately, these myths come from somewhere and sometimes this can be providers that our patients have interacted with previously. While their intentions are likely good, some providers are simply not up to date on the facts about the various contraceptive methods. The internet doesn’t help either. We will never be able to get our patients to stop googling their health questions, but maybe we can provide them with accurate fact sheets and resources so that they can educate themselves.
What are some of the common myths?
 Oral Contraceptive pills (OCPs):
Oral Contraceptive pills (OCPs):
The pill causes weight gain
Many studies have shown that OCPs do not cause weight gain. Weight that is gained while a patient is on OCPs is likely due to external factors. Encouraging regular exercise and a healthy diet and lifestyle is always important.
The pill should not be taken by women who smoke, have diabetes, or are obese
According to the Centers for Disease Control (CDC) a smoker should not use OCPs if she is 35 years of age or older and smokes 15 or more cigarettes a day. Most diabetics can use OCPs. If their diabetes is complicated or if they present with multiple cardiovascular risk factors, then other methods should be considered.
Monthly bleeding is needed with the pill
Explaining to patients how the pill works is important. Let them know that because the endometrial lining is being thinned out by the hormones, they do not need to have their period every month. Lack of menses is not concerning because we know why they are not menstruating. The endometrium is not proliferating uncontrollably.
The pill reduces a woman’s fertility
After stopping OCPs and once the ovulatory cycle has returned to normal, there is not a negative effect on fertility. In fact, the risk of primary infertility may actually be reduced in women who have taken OCPs.
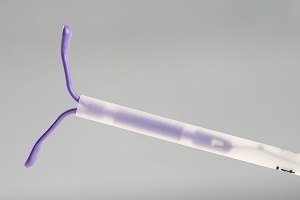
IUDs increase the risk of infection
Placement of the IUD carries a small risk of post-procedure infection. Women are screened and treated for sexually transmitted infections prior to insertion for this reason.
IUDs should not be used in women who have not been pregnant
There are no contraindications to IUD placement in a woman simply because she has never been pregnant. There are many providers who believe that lack of pregnancy means that a patient should not get IUDs. The Skyla and Kyleena IUDs are slightly smaller than Mirena, Liletta, and Paragard and may fit more easily in a nulliparous uterus, but all the IUDs can be placed in women who have not been pregnant.
IUDs increase the risk of ectopic pregnancy
IUDs significantly decrease the risk of ectopic pregnancy. However, if the patient does become pregnant with an IUD, it is more likely that it will be an ectopic pregnancy.
IUDs cause abortions
Hormonal IUDs work by thickening the cervical mucus to prevent the sperm from entering the uterus, they thicken fluid in the fallopian tubes to prevent the egg and sperm from meeting, and thin the lining of the uterus so that if the sperm and egg meet, they cannot implant. The copper IUD creates a localized inflammatory reaction in the uterus that acts as a spermicide and makes the environment unfriendly so that a fertilized egg cannot implant. If a fertilized egg implants in the uterine lining, the IUD will not cause the pregnancy to terminate.
Educating Patients
Overall the benefits of contraception outweigh the risks. Educating patients about how their contraceptive method works and what the facts are is not only empowering for them, but can also help them find the method that is right for them and continue with it. If women know how their contraceptive method works, and they are happy with it, they’ll likely talk to their friends about it. Hopefully this will help spread accurate information. A great patient friendly and accurate contraception website is Bedsider!
Sources:
Hatcher, R. A., Trussell, J., Nelson, A. L., Cates, W., Jr., Kowal, D., & Policar, M. S. (2011). Contraceptive technology. New York, NY: Ardent Media.